Local physicians are doing their part to turn the tide of the opioid epidemic.
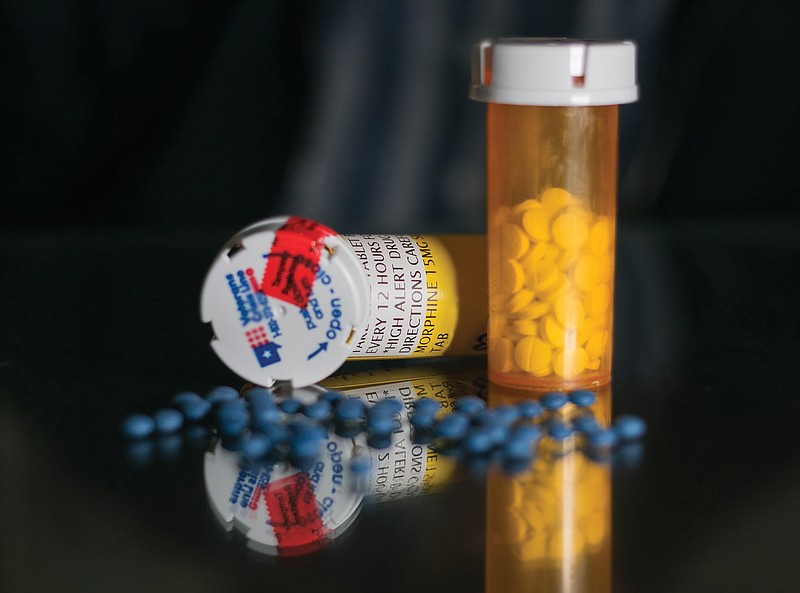
Opioids, opium-like compounds that bind to one or more of three opioid receptors in the human body, are often prescribed to help people deal with severe pain from injury or surgery. And while they work well to manage or eliminate pain, they also create a feeling of euphoria in many users that can lead to misuse and addiction.
"I think the whole epidemic was started by us as providers wanting to give relief to our patients, and unfortunately, that's probably been carried a little too far," said Dr. Matt Young, medical director and physician owner of Texarkana Emergency Center. "With that said, we as providers want to make sure our patients are comfortable. We also need to make sure we're giving them the appropriate medication that we feel is right for their injury or surgery. Our job as a provider is to try to manage patients' expectations and relieve pain. We are all for that, but it's a matter of caring for the patient as a whole patient, and that means trying to prevent them from getting into addictive habits."
Opiates are a valid option for treatment in certain situations.
"There is still a valid place in medicine for acute pain patients, especially post-surgical, to utilize opioid therapy," said Dr. Matthew Johnson, an interventional pain management specialist with CHRISTUS Trinity Clinic. "As an anesthesiologist, these are used quite often to control a patient's pain for the first two or three days after surgery when the pain is deemed the most intense. There is definitely still a place for them, just not in the manner they were originally prescribed."
Opiate prescriptions started increasing in the 1980s and '90s, but as the risk of addiction became apparent, the trend has changed.
"Opioid therapy has lost favor in more recent years," Johnson said. "Opioid treatment for chronic pain has fallen out of favor compared to as early as five years ago, (when) it was the treatment of choice. Back then, a patient would come in, (and) you'd give them a healthy supply of narcotics for lower back pain or headaches.
"As we've evolved in our understanding of how that affects patients long term, we've come up with better modalities to treat pain. We've gotten out of putting patients on long-term opioid therapy versus seeking other options. Patients were just following doctors' orders, and doctors were going on what they had available to them. If a patient came in with back pain, they got narcotics. Patients were treated in this manner for years. Now, we've assessed and see the physical and psychological ramifications, and we have to take a stance against it."
When people take opiates on a regular basis, they have to increase the dosage to get the same pain relief or the same euphoric feeling.
"The longer you use them, the less receptors you have available. You'll have an alteration in response to the medication, and you'll develop a tolerance to those medications. Dependence and addiction can ensue from these. The release of endorphins becomes less and less over time, so you require more and more to get that high back," Johnson said.
Though Johnson still sees opioid therapy as useful, how to use them is still up for debate.
"There is considerable debate in this field. When do you start? How long do you prescribe them for, and what candidates would be most appropriate to utilize opioid therapy?" Johnson said. "In my clinic we have opioid therapy specifically for patients with chronic, degenerative cancer pain. I can count on one hand how many patients fit that criterion. The number has shrunk tremendously."
Better communication between physicians and patients is one way the medical providers are addressing the opioid crisis.
"Without a doubt the community of patients and community of providers have increased their knowledge of the addictive nature of opioids," Young said. "It's incumbent for providers to have that conversation that there's an acute amount of pain we'll treat with opioids after a surgery or injury, but after that, we'll have to transfer you from an a opioid to another medication to help you with the pain, but also help with life. It's a group effort. We're all trying to achieve the same goal, and that's to get the patient back to being at their optimum."
Lower back pain is one of the most common types of chronic pain, making up 70 t0 80 percent of the patients Johnson sees.
Instead of handing out a dangerous prescription, doctors are looking for other ways to treat pain, including spinal injections, physical therapy and nerve ablation.
"I typically don't prescribe any medications for these patients. I'm very much an interventionist. If patients ask for immediate relief, I tell them to take over-the-counter NSAIDs or Tylenol. I try to keep it within that circle," Johnson said.
Empowering people to improve their health and pain level is also important.
"I wish we had a magic bullet or a magic pill to take away all their pain, but unfortunately, we don't have that available to us. What I try to express to patients is if they're at a certain place and they're trying to get to another place, if their physical activity isn't where they want it to be, it doesn't mean we can't get you there with work and discipline," Johnson said.
Physical therapy, aqua therapy and weight loss are tools patients can use to safely decrease pain levels, and the field of pain intervention is evolving.
"From a pain-management perspective, we've been doing epidurals and injections for 30 years. It's not all pain doctors do now days. The field is rapidly growing and expanding. Options for patients are much better than they were even five years ago. The technology to treat people with low-back and leg pain is improving on a monthly basis. Don't give up hope. There's always help out there for you in some form or fashion," Johnson said.
Addiction to opioids is a widespread problem locally with no easy answer.
"It affects everyone in our community," Young said. "It's all social classes, all ethnic groups. Everyone we know has been affected by this in some way or another, and it is problematic. That is why physicians are trying to be part of the solution and not part of the problem."
Statistics from the National Institute on Drug Abuse:Since 2007, overdose deaths due to heroin have increased.
More than 90 people die every day in the U.S. after overdosing on opioids.
The CDC estimates opioid misuse has a $78.5 billion price tag each year when it comes to health care, lost productivity, addiction treatment and criminal and justice involvement.
In 2015, more than 33,000 Americans died of opiod overdose and an estimated 2 million people suffered from substance use disorders related to prescription opioids.
About 21 to 29 percent of patients prescribed opioids for chronic pain misuse them.
About 8 and 12 percent develop an opioid use disorder.
It's estimated that 4 to 6 percent of people who misuse prescription opioids transition to heroin.
About 80 percent of people who use heroin first misued prescription opioids.